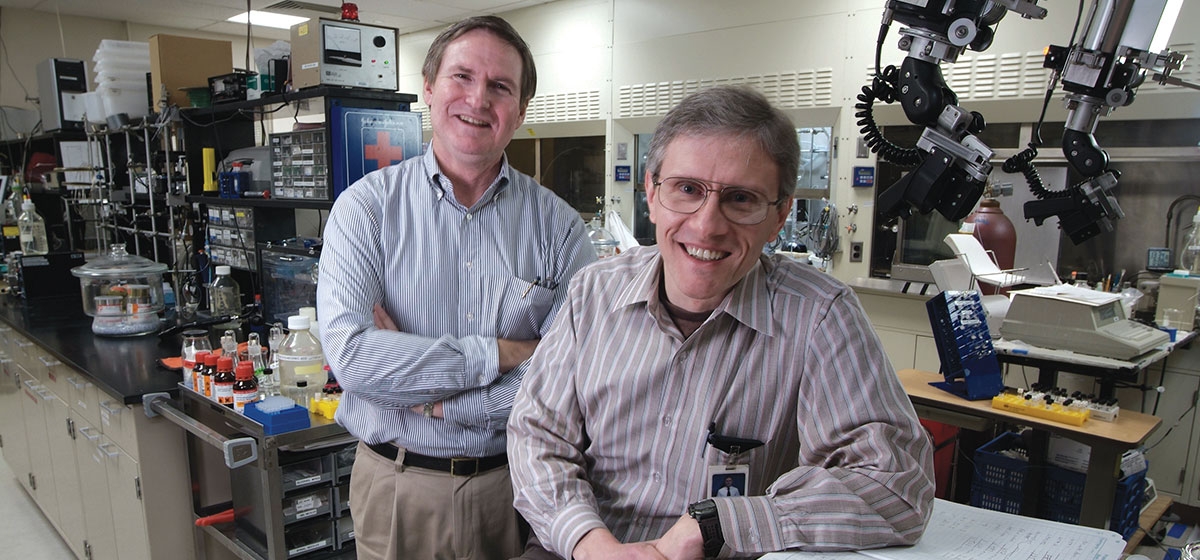
For five years, Chet Mathis, fellow University of Pittsburgh scientist Dr. Bill Klunk and a team of chemists designed hundreds of chemical compounds looking for one that would open the door to the discovery of a drug capable of taming Alzheimer’s disease.
For five years, their lab work and chalkboard theories bought them a few fleeting moments of promise, but little else.
Their fortunes were about to change.
The day’s light was fading outside UPMC Presbyterian Hospital’s ninth floor positron emissions tomography (PET) laboratory, where Mathis was working late. It was mid-autumn, 1999. A new compound conceived from years of trial and error had been injected into a mouse earlier that day. Mathis fetched the numerical descriptions of events that had occurred inside the creature’s brain and began to read.
It was a Eureka! moment, but Mathis had learned to temper optimism. His first word was, “wow.”
“I knew without even working through the arithmetic that it was so much better than anything else we had tried,” says Mathis, Ph.D., director of the university’s PET facility.
The numbers told him that significant amounts of the compound, a derivative of a dye called Thioflavin T, had slipped into the brain of a mouse, eluding the brain’s stingy defenses far better than any of the other compounds they had built.
By getting the dye “in brain” so well, they overcame one of the biggest obstacles blocking the discovery of a chemical compound that, used with a PET scan, vividly displays evidence of beta amyloid, a microscopic protein fragment suspected by many to be a cause of Alzheimer’s.
Today, a close relative of that compound – Pittsburgh compound B – has been proven safe, effective and ready to use in living patients. And it has brought Mathis and Dr. Klunk a host of honors and wide recognition in their field – all for good reason.
Until Pittsburgh compound B, scientists experimenting with promising anti-amyloid drugs to stave off Alzheimer’s lacked a quick, precise way of telling how well they worked in the brains of the living. Now, with such a tool, laboratories not only have an accurate measuring stick, but they should be able to significantly shorten the time it takes to develop the new drugs, which are big reasons why many experts are hopeful about the chances of controlling the disease sooner rather than later.
“I am absolutely convinced we will see medications that will change the course of the disease in the foreseeable future,” says William H. Thies, Ph.D., vice president of medical and scientific affairs at the Chicago-based Alzheimer’s Association. “Whether it’s in three, five, eight or 12 years, I’m not smart enough to tell you. But I think we will get to a stage where Alzheimer’s will become a manageable chronic disease.”
The stakes are high.
When baby boomers reach their seventies, Alzheimer’s disease could afflict nearly 14 millions Americans. The work led by two researchers ~ and now used by dozens of laboratories all over the world ~ will change the course of the disease.
Alzheimer’s is a debilitating brain disorder that ultimately leads to death. It starts with mild memory loss, changes in personality and a decline in the ability to think, then robs patients of speech and movement before rendering them completely incapacitated.
If the disease remains unchecked, when the baby boomers reach their seventies it will afflict an estimated 14 million Americans and cripple the nation’s economy. In 2002, when 4.5 million Americans had the disease, the cost of their care soared above $100 billion. Alzheimer’s-related costs borne by businesses alone exceeded $61 billion, according to an Alzheimer’s Association study. Federal Medicare and Medicaid programs already spend more on Alzheimer’s care than any other disease. Then there is the question of who will care for such a large, very needy patient population when the elderly begin to outnumber the young.
“Now is the time we need to find these therapies because the number of people who are going to get demented will be immense,” says Dr. Steven T. DeKosky, director of the Alzheimer’s Disease Research Center at the University of Pittsburgh.
The good news is that scientists do not have to discover a cure for Alzheimer’s to prevent such gloomy forecasts from becoming reality. They need only to delay its onset. For the most part, Alzheimer’s is a disease of the elderly with most cases occurring after age 75. The math suggests that delaying onset by five years would cut the prevalence of the disease in half over a few decades. Delaying onset by 10 or more years could eliminate it as a major health concern.
The prospects of that happening have brightened considerably since 1984, when the federal government began funding a network of research centers to solve the mysteries of Alzheimer’s. Pitt’s Alzheimer’s Disease Research Center was among the first 10 funded. Today, there are 30.
The centers are the nerve center of Alzheimer’s research in the U.S., gathering and sharing everything from brain tissue to data, educating physicians and researchers and exploring the disease from many angles. They play a key role in clinically evaluating current drugs that treat Alzheimer’s symptoms, such as memory loss, while leading efforts to develop a new generation of therapies that change the course of the disease and stop its relentless march through the brain.
“They’ve been responsible for most of the big science in Alzheimer’s disease,” says Dr. DeKosky, who has been in the thick of the national research campaign for 20 years. “When they started, nobody knew much about this disease. The idea that you could develop a therapy was fantasy.”
Scientists are not certain what causes Alzheimer’s disease. But they know that the brains of Alzheimer’s patients hold an abundance of two abnormal structures: plaques, caused by a buildup of beta amyloid protein, and tangles of threadlike fibers, which result from changes in a protein called tao.
The prevailing hypothesis among scientists casts beta amyloid as the primary cause of the disease and assigns tao a co-starring role. Evidence supporting that idea includes the fact that people with Down syndrome carry an extra copy of the amyloid gene and most develop brain plaques and symptoms of Alzheimer’s, usually by middle age.
Pittsburgh compound B was wedded to the amyloid hypothesis from the beginning.
Dr. Klunk, 49, came to Pitt in 1984 from Washington University in St. Louis after finishing an M.D.-Ph.D. program in neuroscience. When he first met Mathis in 1994, he had begun a project to identify beta amyloid in the brain using derivatives of a dye called Congo red. Mathis, 56, had joined the PET lab two years earlier. He, too, had worked with the Congo red dye, labeling it with radioactive isotopes as a chemist at California’s Lawrence Berkeley National Laboratory, where scientists were also looking at a way to mark amyloid in the brain.
The two hit it off immediately. “Congo red came up in conversation and Bill was surprised I knew of it and had actually worked with it,” says Mathis.
Intrigued by Dr. Klunk’s project, Mathis signed on. Not only did Dr. Klunk have another experienced investigator in the fold, he gained access to PET, which offers a more detailed picture of the brain than the magnetic resonance imaging scans he had been using.
They would start by drawing a chemical structure on the chalkboard, then discuss ways of changing this atom or that to see if they could build a compound with the properties they felt it needed. First, the compound had to sneak safely and effectively past the brain’s defenses. Once inside, it had to stick to amyloid and only amyloid. It had to clearly distinguish amyloid from everything else in the brain. And it had to quickly clear out of the brain once the job was done. The best compounds were injected into mice and the most promising of mouse studies moved on to primates.
More than 250 Congo red derivatives were made over five years, but fewer than 20 percent were good enough to study in mice and only one percent ever made it to primates. None was promising enough to recommend for testing in humans.
Mathis had several other projects on his plate at the PET lab and this one, he admits, was on the back burner for a few years. Dr. Klunk, who had invested much of his research time in the Congo red project, had more reason to worry about the lack of results. The coins of the realm in academia are research papers and grants. Failing to find a suitable dye would leave him with precious little to publish for all of the years and money spent on the investigation.
“I had senior investigators warn me that it was a very high-risk project,” says Dr. Klunk, director of psychiatry at Pitt’s Alzheimer’s Disease Research Center. “But it was the one that interested me the most. And having a Ph.D. helped. I thought that if it all fell apart, I could be a clinical psychiatrist and feed the family that way.”
Soon after switching their focus to the Thioflavin T dye, the prospects of success improved. Early derivatives bound well to amyloid. That autumn evening in 1999 proved that eliminating the compound’s positive charge allowed it to steal past the brain’s defenses. Although it would not clear out of the brain once it stuck to the plaque, the team knew from experience how to fix that problem.
They tinkered for another 18 months, testing some 20 Thioflavin T derivatives for one that had all of the properties it needed to become a powerful tool in the war against Alzheimer’s. The final refinement was tweaking the compound so that it would more vividly distinguish amyloid plaque from other brain tissue on a PET scan.
On Valentine’s Day 2002, researchers at Uppsala University in Sweden phoned to say that Pittsburgh compound B had safely and clearly pinpointed amyloid plaques in the brains of 16 Alzheimer’s patients tested. Says Mathis, “That was when I knew, OK, we got it.”
Today, dozens of laboratories in the U.S., Europe, Asia and Australia are using Pittsburgh compound B in studies of living Alzheimer’s patients. The Pitt researchers, for example, recently used the compound to map the regions of the brain where amyloid plaque first develops and the routes it takes as Alzheimer’s progresses.
More important contributions to the race to conquer Alzheimer’s lie ahead. The compound will soon be used by several labs to determine whether new drugs that interfere with the buildup of amyloid plaque slow, stop or reverse the course of the disease, as many scientists predict. “It is immensely significant for speeding up the development of these anti-amyloid therapies,” says Dr. DeKosky. “That’s why Bill Klunk and Chet Mathis worked so hard to put it together.”